CLIA CMV IgG BioVendor Group Instruction Manual
- June 13, 2024
- CLIA
Table of Contents
CLIA CMV IgG BioVendor Group

Product Information
- Product Name: CLIA CMV IgG
- Product Code: CL-CMG100
- Intended Use: Kit for professional use in the diagnosis and screening of CMV infection using IgG antibodies in human serum or plasma in the general population.
- Test Principle: The kit utilizes purified and inactivated antigen isolated from CMV AD 169 strain with a high content of specific immunodominant epitopes.
Product Usage Instructions
- Storage and Stability: The kit should be stored at the recommended temperature and protected from light. Refer to the user manual for specific storage instructions.
- Preparation of Reagents: The kit provides reagent cartridges, sample diluent buffer, conjugate solution, and calibrators. These reagents are ready to use and do not require any additional preparation.
- Quality Control: Perform quality control procedures as described in the user manual to ensure accurate and reliable test results.
- Test Procedure: Follow the step-by-step instructions provided in the user manual for performing the CMV IgG test using the provided reagents and calibrators. This includes sample preparation, cartridge loading, incubation, washing, addition of conjugate solution, reading the results, and interpretation.
- Result Interpretation: Refer to the user manual for detailed information on how to interpret the test results. The manual provides guidance on differentiating between primary infection and reactivation based on IgG antibody levels and avidity.
- Analytical Performance: Consult the user manual for information on the analytical performance of the CMV IgG test, including sensitivity, specificity, precision, and accuracy.
- Clinical Performance: Refer to the user manual for data on the clinical performance of the CMV IgG test, including its diagnostic accuracy in different populations.
Safety Precautions:
Follow the safety precautions outlined in the user manual to ensure safe
handling of the kit and proper disposal of materials.
Procedural Notes:
Take note of any specific procedural considerations or recommendations
provided in the user manual for optimal test performance.
References:
The user manual provides a list of references for further reading and
verification of the test methodology and performance.
Document Records
| Revision No. | Version No. | Revision Description |
|---|---|---|
| 0 | 1 | New Document |
Intended Purpose
The chemiluminescence assay is intended for the diagnosis and screening of
CMV infection using IgG antibodies in human serum or plasma in the general
population. The quantitative automated assay is designed for professional use
in a laboratory
Introduction
Human cytomegalovirus (CMV, Human Herpesvirus 5, HHV 5) belongs to the group of herpesviruses.
Primary infection with human CMV most commonly occurs in childhood or adolescence via various modes of transmission (respiratory, urogenital). The clinical course is usually asymptomatic or mild (fever, fatigue, symptoms of mononucleosis). After primary CMV infection, the virus enters a latent phase and subsequent reactivation (secondary infection) occurs depending on changes in the host- virus relationship (pregnancy, severe illness, stress, immunosuppressive therapy). Reinfection may occur with another CMV strain. Primary CMV infections during pregnancy pose a serious risk (congenital infections with varying degrees of damage occur in 1/3 to 1/2 of newborns, while only in 1% in case of reactivations). Immunocompromised people (AIDS, transplants, etc.) usually develop symptoms with involvement of various organs, often with fatal consequences.
The diagnosis of the disease is based on clinical picture and laboratory tests. Serological methods for the determination of specific IgA, IgM and IgG class antibodies are most commonly used in the laboratory diagnosis of CMV. IgA antibodies are an indicator of active infection, i.e. primary infection and reactivation. Reactivation produces antibodies of the IgA class, which may or may not be accompanied by specific IgM. Thus, IgA class antibodies are of great importance for the confirmation of CMV reactivation in the presence of IgG antibodies.
IgM antibody levels usually increase several weeks after the infection and then slowly decrease over 4 to 6 months. In immunodeficient patients, they may be present at low levels for up to two years after infection. The detection of IgM antibodies alone cannot distinguish between primary and secondary infection, as reactivation can also induce their synthesis. Specific IgG antibodies are detectable approximately 1 week after the increase of IgM and IgA levels. Their seroconversion (titre increase) indicates primary infection. The differentiation of primary infection from reactivation is based on the avidity of IgG antibodies, which is important for the assessment of the risk of congenital infection.
Detection of IgG antibodies is also established as a standard method for identifying CMV positive individuals in donor screening.
Test Principle
The kit is intended for the detection of specific antibodies in a sample
using the CLIA method (Chemiluminescence Immunoassay) on KleeYa®, STRATEC SE.
The solid phase consists of magnetic particles with a specific antigen the
antibody from the tested sample binds to. Subsequently, binding occurs with
the conjugate-labelled antibody. The labelled antibody is an animal anti-human
immunoglobulin fraction conjugated to a chemiluminescent agent (acridinium
ester). When oxidized with hydrogen peroxide in an alkaline environment, the
acridinium ester emits light. The light intensity is measured with a
photomultiplier in relative light units (RLUs) and is proportional to the
concentration of specific antibodies in the sample.
-
Antigen Used
Purified and inactivated antigen isolated from CMV AD 169 strain with a high content of specific immunodominant epitopes -
Kit Concept
**** CLIA kits are specifically designed for automatic analysis using the KleeYa® instrument, STRATEC SE. To perform analysis on the instrument, follow the KleeYa® User Manual.
Material Provided
The kit contains cartridges with reagents and calibrators
REAGENT CARTRIDGE
| Magnetic Particles
Coated with antigen, suspension ready to use
|
1 × 5 ml
---|---|---
Sample Diluent
Buffer with protein stabilizers, ready to use
|
3 × 10 ml
Conjugate
Solution containing acridinium ester labelled animal immunoglobulin to human antibodies, ready to use
|
1 × 10 ml
CAL 1| Calibrator 1
Solution containing specific human antibodies, ready to use
|
3 × 1 ml
CAL 2
| Calibrator 2
Solution containing specific human antibodies, ready to use
|
3 × 1 ml
| Calibration sheet
Calibrator identification card containing the calibration (master) curve
|
1 pc

Other Material Required for Test Performance
Table 1 Material and equipment
| Equipment | Catalogue number | Manufacturer |
|---|---|---|
| Trigger pack | 10111184 | Diatron MI Plc. |
| Wash solution (5 × TBS Wash Buffer) | 10111002 | Diatron MI Plc. |
| Disposable tips (Anchor®Tip, 300 µl) | 10036506 | STRATEC Consumables GmbH |
| Cuvettes (Stackable Cuvette, 1 ml) | 10033666 | STRATEC Consumables GmbH |
Trigger Solution 1 a Trigger Solution 2 (Trigger pack) are used to oxidise the acridinium ester resulting in the emission of light.
Storage and Stability
Store the kit at +2°C to +8°C. If the kit is stored as described, the
labelled expiration date is valid. The expiration date is indicated on the
package. The opened kit should be used within three months. Do not freeze!
Sample and their storage
- Samples listed in the intended use may be used for the examination. Samples that are bacterially contaminated, haemolytic or chylous, and anticoagulants contained in plasma (except for citrate) may affect the test result.
- A coagulating blood collection tube is recommended for serum collection. A citrated plasma collection bag is recommended for plasma collection. Other types of plasma (EDTA, heparin) may be used but they are not recommended since anticoagulants may affect the test result.
- Follow the manufacturer’s instructions when using commercial or other specially modified samples.
- Clinical samples collected within standard medical procedures into standardized tubes are ready for immediate use. Centrifugation or other separations are not required.
- The examined samples can be stored at +2 °C to +8 °C for a maximum of 1 week.
Preparation of the Kit for Analysis using the KleeYa®
Instrument
For analysis on the KleeYa® instrument follow KleeYa® analyzer manual. The
result of the first test is available in 30 minutes.
Preparation of Reagents
Dilute the Wash solution (5 × TBS Wash Buffer) 1:5 (1 volume unit of the
solution with 4 volume units of distilled water). E.g., 2 l of concentrated
Wash solution + 8 l of distilled water. The diluted Wash Solution is stable
for one month (on board). The Calibrators are ready to use, do not dilute
further!
All reagents in the Cartridge are ready to use, do not dilute further!
Interchangeability of Reagents
The Wash solution (5 × TBS Wash Buffer), Trigger Solution 1 and Trigger
Solution 2 are universal for all kits.
Quality Control
The test is valid if the calibration curve is accepted. Calibration must be
performed once every 14 days. If the calibrator result is outside the
acceptable range, please contact the Technical Support Department.
You can use your own or externally supplied control material to verify the functionality of the test.
Result Interpretation
Quantitative Evaluation in Units (U/ml)
The level of antibodies (U/ml) in the samples is calculated by the device
based on the calibration curve for the batch. The interpretation of the
results of quantitative test evaluation is given in the Table 2.
Table 2 Quantitative interpretation in Units (U/ml)
| Antibody level (U/ml) | Evaluation |
|---|---|
| lower than 18 | negative |
| 18 to 22 | borderline |
| higher than 22 | positive |
Examination of borderline samples should be repeated from a new sample collected after 2 to 6 weeks regarding to the disease specifics. Serological finding can be interpreted only in the context of results of other laboratory tests and patient clinical picture.
Analytical Performance
Specificity and Sensitivity
Specificity was determined in the panel of negative samples. Sensitivity
was determined in the panel of positive samples. The number of samples tested
and the results obtained are described in the table (Table 3).
Trueness (bias)
Trueness is the closeness of agreement between the average value obtained from
a large number of measurement results and the reference value. Its measure is
bias. The nature of the method does not allow quantitative determination of
bias (and thus the trueness). The trueness of the method is ensured by
clinical parameters such as sensitivity and specificity, comparison with the
reference method and batch continuity. The obtained results are described in
the table (Table 3).
Precision: Repeatability – Intra assay (within run)
The precision is defined as the closeness of agreement between measured
values obtained by replicate measurements on the same object under specified
conditions. The Intra-assay repeatability is expressed as agreement level
among sample replicates within a run of the assay (in one batch). The obtained
results are described in the table (Table 3).
Precision: Reproducibility (within-laboratory, between-day, between-run)
Reproducibility is a measure of precision under a defined set of conditions which include the between-day and between-run components and the within- laboratory precision, expressed as the agreement level among sample replicates measured in different testing days and runs. The obtained results are described in the table
Accuracy
Accuracy is defined as the closeness of agreement between the measured
value and the reference value. It is expressed as an achievable measure of the
combined uncertainty. The obtained results are described in the table (Table
3).
Analytical sensitivity – limits of detection and quantitation
The analytical sensitivity is the maximum binary dilution of CUT-OFF-like
serum or international standard sera, respectively, giving signal intensity
(expressed in RLU, Relative light units) different from the background. The
difference in mean RLU compared to the previous dilution is less than 5 %.
The value is expressed as a concentration in units. This value is a minimum
limit of detection. The obtained results are described in the table (Table 3).
Measuring Range
The measuring range of the assay lies between the values 0,1–160 U/ml.
Linearity
The linearity is the ability of the method to obtain final values
proportional (directly or after mathematical transformation) to the
concentration of analyte in the sample; it is expressed as the range in which
the method provides linear results. The obtained results are described in the
table (Table 3).
Hook effect
Hook effect is an immunological phenomenon that causes falsely low results in
the presence of an excess amount of analyte. Its presence is detected by
serial dilution of a highly positive sample (Table 3).
Comparison with the reference method
Comparison with the reference method was performed. The results of both
methods are comparable, considering the differences of both methods and
completely meeting the requirements if the agreement in the classification of
the samples is at least 90% (Table 3).
Table 3 Analytical Performance
| Parameter | Value |
|---|---|
| Sensitivity (n 119) | 98.31% |
| Specificity (n 60) | 98.33% |
| Trueness (bias) | N/A |
| Precision: Repeatability | 6.56% |
| Precision: Reproducibility | 12.94% |
| Accuracy | 14.88% |
| Analytical sensitivity | 0.67 U/ml |
| Measuring Range | 0.1–160 U/ml |
| Linearity interval | 14.21–181.62 U/ml |
| Hook effect | Not observed |
| Comparison with the reference method | At least 90% |
Interference
Two samples (one negative plasma pool and one positive plasma pool) were
spiked with potentially interfering substances. Results of interference
testing are shown in the table (Table 4).
Table 4 Interference Results
Interfering substance
| The result was not affected up to concentration:
---|---
Bilirubin| 0.4 mg/ml
Triacylglycerols| 20 mg/ml
Haemoglobin| 5 mg/ml
Biotin| 3500 ng/ml
Cross-reactivity
The assay was evaluated for potential cross-reactivity using samples positive
for selected pathogens and factors. Results of testing are shown in the table
(Table 5).
Table 5 Results of Cross-Reacting Pathogens or Factors
| Category | (n) | Positive result |
|---|---|---|
| EBV VCA | 7 | 1 |
| HSV 1+2 | 7 | 0 |
| VZV | 8 | 0 |
| Rubella virus | 8 | 0 |
| Toxoplasma gondii | 3 | 0 |
| Measles virus | 6 | 0 |
| Mumps virus | 6 | 0 |
| Mycoplasma pneumoniae | 5 | 0 |
| Total | 50 | 1 |
Clinical Performance
Diagnostic specificity and diagnostic sensitivity
Diagnostic specificity has been established on a panel of negative samples.
Diagnostic sensitivity has been established on a panel of positive samples.
The number of samples tested and the results obtained are shown in the table
(Table 6).
Positive and negative predictive value
A positive predictive value is probability that a person is actually affected
by infection if the result was positive. A negative predictive value is
probability that a person is actually healthy if the result was negative. The
results obtained are shown in the table (Table 6).
Likelihood ratio of the kit
The likelihood ratio of the kit for a positive test is the ratio of
probability that an individual from affected population is diagnosed as
positive by the test and probability that a healthy individual is misdiagnosed
as positive. The likelihood ratio of the kit for a negative test is the ratio
of probability that an individual from affected population is misdiagnosed as
negative by the test and probability that a healthy individual is diagnosed as
negative. The results obtained are shown in the table (Table 6).
Expected values in population
Expected values in population are established based on the value results in a
file of samples declared as negative and a file of samples declared as
positive for the presence of specific antibodies. The results obtained are
shown in the table (Table 6).
Table 6 Clinical performance
| Parameter | Value | 95% Confidence Interval (CI) |
|---|---|---|
| Diagnostic sensitivity (n 119) | 98.31% | 94.01–99.79% |
| Diagnostic specificity (n 60) | 98.33% | 91.06–99.96% |
| Positive predictive value (n 119) | 99.15% | 95.33–99.98% |
| Negative predictive value (n 60) | 96.72% | 88.65–99.60% |
| Likelihood ratio of the kit for a positive test | 58.983 | – |
| Likelihood ratio of the kit for a negative test | 0.017 | – |
| Expected values in healthy population | 6.68 U/ml | 5.44–7.92 U/ml |
| Expected values in affected population | 293.74 U/ml | 250.16–337.32 U/ml |
Safety Precautions
The kit is intended for in vitro diagnostic use only. The sera used for controls were tested and found to be negative for HIV 1 and HIV 2, HBsAg, HCV, TPHA. In spite of this fact, they still need to be handled as potentially infectious materials. Some reagents contain the toxic component sodium azide in very low concentrations. Avoid contact with skin. Local work safety regulations must be observed.
First Aid
In case of contact with eyes, flush with copious amount of water and seek
medical assistance. In case of contact with skin and clothing, remove all the
contaminated clothes. Wash the skin with soap and plenty of running water. In
case of contact with solutions containing plasma or clinical samples,
disinfect the skin. In case of accidental ingestion, flush the mouth with
drinking water and seek medical assistance.
Remnants Disposal
All the materials used for performing the test must be treated as potentially
infectious due to the contact with biological materials. Therefore, they need
to be disposed together with biological waste.
Expired Kit Disposal
Disassemble the kit and dispose the components as biological material. Discard
the packaging material as required by local regulations.
Procedural Notes
In order to obtain reliable results, it is necessary to strictly follow the
Instructions for Use. Always use clean preferably disposable tips and
glassware. Wash Solution – use high quality distilled water for preparing the
working strength Wash Solution.Non-reproducible results might be caused by
improper methodology as following:
- insufficient mixing of reagents and samples before use
- improper replacement of vial caps
- reagent exposure to excessive temperature; bacterial or chemical contamination
- using reagents from different kit lots
- contact of reagents with oxidants, heavy metals and their salts
Technical limitation of samples
Materials of a human origin from donor population listed in the intended use
were used for manufacture and development of the kit. Kits are intended for
use in general population, unless otherwise stated. When using samples from
other specific populations (comorbid, immunocompromised, pregnant, paediatric
population), the risk of a specific effect on the result of the applied test
due to e.g. interference or cross-reactivity should be considered in the
context of expert knowledge and current scientific knowledge.
Other notes
The kit might be used for sequential examinations. The kit can be used only on
the KleeYa® analyzer
References
- Blackburn NK, Besselaar TG, Schoub BD, O΄Connell KF. Defferentiation of primary cytomegalovirus infection from reactivation using the urea denaturation test for measuring antibody avidity. J Med Virol. 1991, 33(1), 6-9.
- Bodeus M, Feyder S, Goubau P. Avidity of IgG antibodies distinguishes primary from non-primary cytomegalovirus infection in pregnant woman. Clin Diagn Virol. 1999, 12(1), 3-8.
- Boeckh M, et al. Quantitation of cytomegalovirus: methodologic aspects and clinical application. Clin Microbiol Rev. 1998, 11(3),533-554.
- Dussaix E, Chamtit S, Harzic M, Grangeot-Keros L. CMV-IgG avidity and CMV IgM concentracion in both immunocompromised and immunocompetent patiens. Pathol Biol. 1996, 44(5), 405-410.
- Grangeot-Keros L, Mayaux MJ, Lebon P, Freymuth F, et al. Value of cytomegalovirus (CMV) IgG avidity index for the diagnosis of primary CMV infection in pregnant women. J Infect Dis. 1997, 175(4), 944-946.
- Joassin L, et al. Elimination of nonspecific cytomegalovirus immunoglobulin M activities in the enzyme-linked immunosorbent assay by using anti-human immunoglobulin. J Clin Microbiol. 1986, 23(3), 576-581.
- Lazzarotto T, Varani S, Guerra B, Nicolosi A, et al. Prenatal indicators of congenital cytomegalovirus infection. J Pediatr. 2000, 137(1), 90-95.
- Pappin A, et al. Stability of cytomegalovirus antibodies in plasma during prolonged storage of blood components. Clin Diagn Lab Immunol. 1995, 2(1), 25-29.
- Revello MG, et al. Diagnosis and Management of Human Cytomegalovirus Infection in the Mother, Fetus, and Newborn Infant. Clin Microbiol Rev. 2002, 15(4), 680-715.
IFU Symbols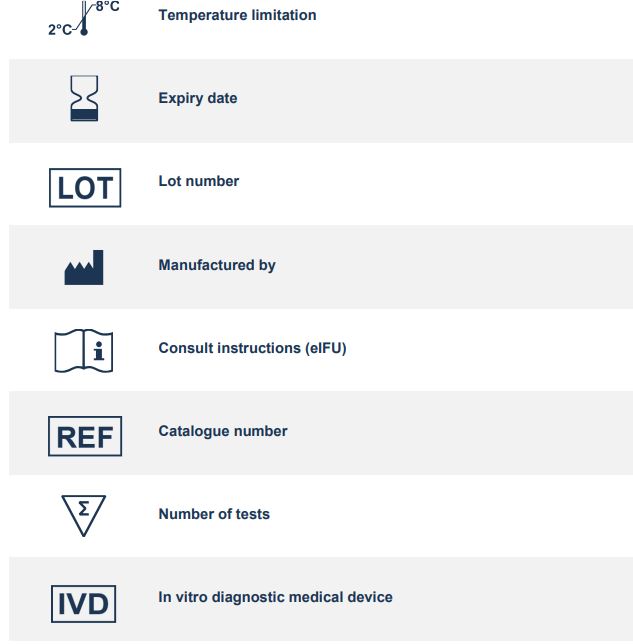
TestLine Clinical Diagnostics s.r.o. Krizikova 68, 612 00 Brno, Czech Republic +420 541 248 311 support.clia@biovendor.group clia.biovendor.group
Read User Manual Online (PDF format)
Read User Manual Online (PDF format) >>